Medical waste (such as contaminated dressings, used syringes, and expired pharmaceuticals) poses a potential threat to public health and environmental safety. According to the WHO, approximately 16 million tons of medical waste are generated globally each year, 15% of which are infectious or sharp wastes. Improper disposal can not only lead to needlestick injuries and pathogen transmission but also result in heavy fines. As a core disposal device, the disinfection standards and operational details of medical waste shredders directly determine the effectiveness of safety risk control. This article provides an in-depth analysis of key points, combining industry cases, technical details, and European and American compliance requirements.
I. Core Value and Technical Logic of Medical Waste Shredders
Medical waste shredders are not ordinary industrial shredding equipment; they are specialized systems designed around "safe inactivation + compliant volume reduction + cost optimization". Their technical logic can be broken down into three dimensions:
1. Volume Reduction and Cost Reduction: From "High-Cost Transportation" to "Efficient Compression"
The disposal costs (transportation, incineration, landfilling) of medical waste are strongly correlated with its volume. Untreated waste has a density of only 0.2–0.3 tons per cubic meter, while shredded waste can reach a density of 0.8–1.2 tons per cubic meter, achieving a volume reduction rate of 60%–90%.
Take a secondary hospital as an example: It generates 200kg of medical waste daily. Without shredding, it requires a 1.5-ton specialized vehicle for daily transportation to an incineration plant, costing approximately $8,000 per month. After shredding, the volume is compressed to 40kg, allowing transportation every 3 days with a 0.5-ton vehicle. Monthly transportation costs drop directly to $2,000, saving $72,000 annually.
2. Risk Control: Eliminating Sharp Objects and Biological Contamination
Sharp wastes (syringes, scalpels) are a major source of needlestick injuries for medical and cleaning staff. According to OSHA data, approximately 380,000 needlestick injuries occur in U.S. healthcare facilities each year, 25% of which are related to improperly handled medical waste.
The blunt-shredding design (cross-shearing of dual-shaft blades) of shredders breaks sharp objects into harmless fragments smaller than 10mm. Meanwhile, enclosed chambers and negative-pressure exhaust systems prevent the spread of infectious aerosols. When paired with built-in high-temperature (200°F for 30 minutes) or hydrogen peroxide spray disinfection modules, shredders can kill 99.99% of pathogens (including hepatitis B virus, COVID-19, drug-resistant bacteria, etc.), cutting off transmission chains at the source.
3. Compliance Adaptation: Meeting European and American Disposal Requirements
The intelligent data modules of shredders automatically record shredding duration, disinfection temperature, waste type, and processing volume. Electronic logs must be archived for at least 5 years and can be directly used for annual regulatory inspections, avoiding compliance risks due to missing records.
II. Practical Case: Shredder Application Upgrade in a U.S. Tertiary Hospital
A 1,500-bed tertiary hospital (with over 5 million annual outpatient visits) faced three key pain points:
1. Prominent Safety Hazards: 8 needlestick injuries to waste handlers and 2 contact infections among cleaning staff occurred annually, leading to a local health department notice.
2. High Disposal Costs: Daily processing of 600kg of medical waste cost over $28,000 per month in transportation and incineration fees.
3. Compliance Pressures: The existing waste disposal process lacked complete records, resulting in multiple rectification orders.
Solution: Dual-Shaft Thermal Disinfection Shredder + Intelligent Sorting System
1. Front-End Sorting Optimization: Two types of collection bins ("sharp/infectious" and "general medical waste") were placed in each department, equipped with smart scanning devices to record the waste-generating department and type.
2. Integrated Shredding and Disinfection: A dual-shaft thermal disinfection shredder was adopted. Sharp waste was fed into the chamber via an automatic conveyor; blades sheared it into 10mm fragments at 120 rpm, while the internal heater raised the temperature to 200°F for 30 minutes, completing shredding and sterilization simultaneously.
3. Backend Connection and Recording: Shredded waste was collected in sealed bins with built-in RFID tags, automatically linking to front-end sorting data. A compliant agency transported it to the incineration plant twice weekly, with full-process data uploaded to the hospital’s HIS system to form a "generation-treatment-disposal" end-to-end record.
Outcomes
• Zero Safety Incidents: No needlestick injuries or contamination spread were reported in 12+ months; healthcare staff safety satisfaction scores increased by 82%.
• Dramatic Cost Reduction: Monthly disposal costs dropped from $28,000 to $8,400 (a 70% reduction), saving $235,200 annually.
• Compliance Achievement: The hospital passed the U.S. CDC’s "Medical Waste Safety Management" Grade A rating and became a state-level demonstration unit.
III. Key Details for Selection and Use
When selecting a medical waste shredder, avoid the mistake of "focusing only on price." Focus on the following dimensions to ensure the equipment matches your scenario:
1. Matching Waste Type to Equipment Function
• Sharp/Infectious Waste: Prioritize dual-shaft/tri-shaft shredders (high shearing force for hard syringes/scalpels), which must include thermal disinfection (200°F+) or chemical disinfection modules (e.g., hydrogen peroxide spray) to prevent pathogen residue.
• General Medical Waste (e.g., contaminated swabs, gauze): Single-shaft shredders suffice but require anti-tangling designs (to prevent soft waste from clogging blades).
• Chemical/Pharmaceutical Waste (e.g., expired IV bottles, contaminated reagent bottles): Use specialized models with 316 stainless steel corrosion-resistant chambers and Class I Div 2 explosion-proof motors to prevent chemical corrosion or explosion risks.
2. Matching Processing Volume to Scenario
• Small Clinics/Community Health Centers (10–50kg/day): Choose compact desktop shredders (3–7.5 HP, no larger than 20×32 inches) that can be placed in medical waste storage rooms.
• Medium Hospitals/Physical Examination Centers (50–300kg/day): Select floor-standing dual-shaft models with automatic feed conveyors (reducing manual waste contact) that support 8 hours of continuous daily operation.
• Large Hospitals/Medical Parks (300kg+/day): Use industrial-grade tri-shaft models with continuous feeding (processing speed up to 110 lbs/minute) and automatic fault alarm functions.
3. Maintenance and Compliance Details
• Daily Maintenance: Inspect blade wear weekly (sharp waste dulls blades;polish or replace if wear exceeds 0.08 inches); lubricate bearings and clean disinfection module nozzles/heating tubes monthly; replace chamber seals quarterly in high-load scenarios (to prevent disinfection gas leakage).
• Compliance Record Management: Retain shredder operation logs (including date, waste type, processing volume, disinfection temperature, operator); back up electronic records to the cloud, and archive paper records for at least 5 years.
• Emergency Handling: Equip NFPA-standard ABC fire extinguishers (for potential flammable waste); develop "equipment failure/leakage" emergency plans and conduct regular drills for operators.


IV. Frequently Asked Questions (FAQ)
1. Can shredders handle radioactive medical waste?
No. Radioactive waste must be disposed of by NRC-licensed specialized agencies. Shredders are only suitable for non-radioactive infectious, sharp, or general medical waste.
2. Can shredded waste be directly landfilled?
It depends on local regulations and equipment functions: If the shredder has a compliant disinfection module (e.g., high-temperature, chemical disinfection) and local environmental authorities permit "sanitized medical waste landfilling," landfilling is allowed. However, most U.S. states require shredded waste to be incinerated to fully eliminate pathogens and hazardous substances.
3. Will shredder energy consumption increase operating costs?
No. Industrial models consume 4–15 kW/h (depending on processing volume), while small models use only 2–5 kW/h (equivalent to a commercial air conditioner). The reduced transportation and incineration costs from shredding are typically 5–10 times higher than energy costs, significantly lowering long-term operating expenses.
4. How to prevent shredder clogging?
Note three points: ① Do not feed overly hard items (e.g., metal instrument cases); ② Cut soft waste (e.g., large gauze pieces) into batches before feeding; ③ Regularly clean blades and feed ports to keep the interior clear.
The disinfection standards and safety risk control of medical waste shredders are core components of healthcare facility waste management. By matching appropriate disinfection modules, selecting equipment precisely, and maintaining it standardized, facilities can meet European and American compliance requirements while eliminating risks like needlestick injuries and pathogen spread at the source. For healthcare settings, mastering these details is not just about proper equipment use—it is a commitment to staff safety and public health.
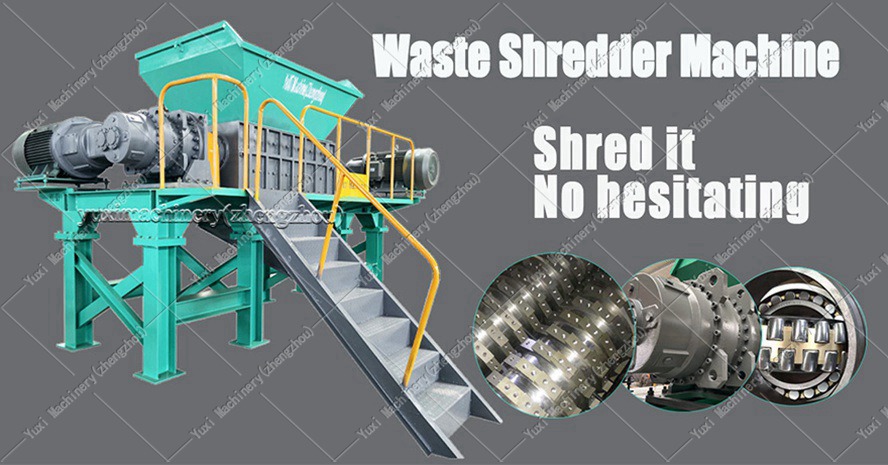
 Shredding Machine
Shredding Machine
 Waste Recycling Line
Waste Recycling Line
 Optional Equipment
Optional Equipment